The Centers for Disease Control and Prevention (CDC) reported that half of all adults has one or more chronic health conditions, and that one of four adults has two or more chronic conditions (Centers for Disease Control and Prevention [CDC], 2012). The chronic diseases that burden the United States (U.S.) healthcare system include heart disease, cancer, type 2 diabetes, obesity and arthritis; these are among the most common, costly and preventable (CDC, 2012). Poor diet, physical inactivity, uncontrolled high blood pressure, tobacco use, and hyperlipidemia, are among the most common modifiable risk factors that are accounting in large part for the current strain on our healthcare system (Bauer, Briss, Goodman, & Bowman, 2014). To successfully and equitably attend to the chronic disease affliction, public health and health-care systems need to employ cohesive approaches that bundle strategies and interventions, produce population-wide changes, address conditions and risk factors concurrently, and rely on implementation by many sectors, private and public alliances and involvement from all stakeholders (Bauer, Briss, Goodman, & Bowman, 2014). A gap in practice exists as it relates to the impacts of patients with chronic conditions on the healthcare system worldwide. The goal of community accountability lead me to the project question: Can a peer-led chronic disease self-management program improve patient outcomes?
Purpose Statement
The primary purpose of this evidence-based Doctor of Nursing (DNP) practice project is to evaluate the effectiveness of a community health based chronic disease self-management program (CDSMP), called "The Healthy Living Workshop." The ultimate goal of the project is to improve patient's management of chronic disease, by ensuring that a community health peer-led group is meeting standards set by the CDC's Framework for Program Evaluation in Public Health. These standards include, (1) utility, (2) feasibility, (3) propriety, and (4) accuracy (CDC, 2016). The results of the study may add the knowledge base of healthcare practitioners to help establish and sustain these educational programs. In addition, the study may help to inform policy makers about the importance of CDSMP.
Objectives
- The project will examine factors associated with acceptance and completion rate of the Chronic Disease Self-Management program.
- The project will highlight the experience of patients, peer leaders, and providers who facilitated the programs.
- The project will help provide outcomes measures for program
Literature Review
The research was conducted using several search engines, including, Cochrane, PubMed, Medline, EBSCO HOST and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) to which peer reviewed, full-text relevant evidence-based data article were acquired. The following keywords were used for this literature search on chronic disease; chronic disease, Stanford university, chronic disease management, self-management programs, self-efficacy, chronic disease self-management programs.
Get Help With Your Essay
If you need assistance with writing your essay, our professional essay writing service is here to help!
The National Center for Chronic Disease Prevention and Health Promotion, which is part of the CDC published an article establishing that chronic disease is a leading cause of preventable death and disability in the U.S. Although non-communicable conditions such as diabetes, cancers, obesity, respiratory and cardiovascular disease account for nearly two-thirds of death worldwide, the U.S leads the world in spending, with close to 96% or $300 billion in support of patients with two or more chronic conditions (Bauer, Briss, Goodman, & Bowman, 2014 ). Data from the National Health Interview Survey found that approximately half of U.S adults or 49.8% has 1 of the 10 most common chronic conditions (ie, hypertension, stroke, coronary heart disease, asthma, arthritis, hepatitis, diabetes, kidney disease, COPD and cancer), with 25.5% having 2 or more conditions (Ward, Schiller & Goodman, 2014). As the complexity of chronic disease management continues to grow, the CDC is partnership with the U.S Department of Health and Human Services (HHS) developed new strategies and intervention divided into four categories, (1) enhanced surveillance, (2) environmental approaches, (3) health system intervention and (4) community-clinical links (Bauer et al., ). Supported alliances between primary care sectors and public health are essential to further develop the community-clinical link framework. This approach will enhance health equity by fostering communities that endorse health rather than disease, bring more availability and direct care into communities, and focus the healthcare system on progressing population health. In addition to building community links CDSMP also show substantial savings over clinician-delivered models and are cost effective (Bauer et al., ).
As mentioned above the care for patients with chronic conditions is a strain on the U.S healthcare system, however analysis of CDSMP programs have shown healthcare saving. Ahn et al. (2013) examined 1,170 CDSMP participants at baseline, 6 months, and 12 months period from 22 different organization in 17 states. Cost savings analysis was conducted, after evaluating six procedures, (1) estimating per participant program costs; (2) ) extrapolating savings to national populations using Census data combined with national health statistics; (3) examining the pattern of healthcare utilization among CDSMP participants from self-reported healthcare utilization assessed at baseline, 6 months, and 12 months; (4) computing potential cost savings by deducting program costs from estimated healthcare savings; (5) calculating age-adjusted average costs for persons using the 2010 Medical Expenditure Panel Survey; (6) calculating costs saved from reductions in healthcare utilization. The results indicated a 5% decrease in emergency room (ER) visits as well as a 3% reduction in hospitalization from baseline to 6-months. This equates to a national savings of $3.3 billion or $364 per participant. Building on this study additional research showed a $38,803 cost saving per participant over a 12-month period (Ahn, Smith, Altpeter, Post, & Ory, 2015) In addition to CDSMP showing cost-effectives through decrease ER visits and hospitalization, incremental cost-effectives ratios have been used to convert quality-adjusted life years to cost savings with ranges from $83,285 to $31,285 in saving per QALYs (Basu et al., 2015).
Theoretical Framework
The CDC's model for program evaluation will be used to best address the clinical issues and the project question: Does a peer-led self-management group focused on chronic condition improve patient outcomes. In addition to the Framework for Program Evaluation the Innovative Care for Chronic Conditions Framework will also be utilized to guide this project. The CDC's Framework for Program Evaluation is designed to be better positioned to detect program validities, and encourage advancement toward outcomes improvement (CDC, 2106). "This program outlines a systematic way to improve and account for program actions, involving methods that are useful, feasible, ethical and accurate. The framework is a practical, nonprescriptive tool, designed to summarize and organize essential elements of program evaluation. The framework comprises steps in evaluation practice and standards for effective evaluation" (Koplan, Milstein & Wetterhall, 1999, p. 6). Following these steps will allow an appreciation for the Healthy Living Workshop's context and will improve how evaluation is imagined and conducted. Elements of the CDC's Framework for Program Evaluation (2016), are (1) engaging stakeholders, (2) describing the program, (3) focusing the evaluation design, (4) gather credible evidence, (5) justify conclusions, and (6) ensuring use and shared lessons learned.
The purposes of the framework are to:
- Summarize the essential elements of program evaluation
- Provide a framework for conducting effective program evaluations
- Clarify steps in program evaluation
- Review standards for effective program evaluation
- Address misconceptions regarding the purposes and methods of program evaluation.
(CDC, 2016)

(Framework for Program Evaluation [Online Image] (2016))
The Innovative Care for Chronic Conditions Framework (ICCC) was adapted from the Chronic Care Model (CCM) in 2002 by the World Health Organization (WHO), to shift the focus from primary care in which the CCM provided to community and policy aspects of improving chronic care. The ICCC framework centers on improving care on three distinctive levels, (1) micro level (family and individuals), (2) meso level (healthcare organization and community), and macro level (policy) (Pruitt et al., 2002).
The Innovative Care for Chronic Conditions Framework
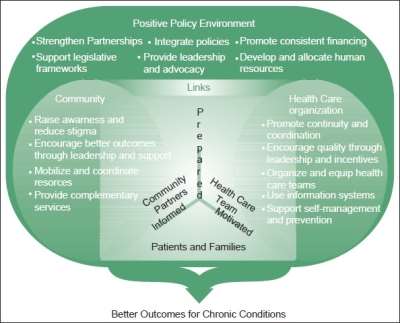
(Innovative Care for Chronic Conditions: Building Blocks for Action [Online Image] (2002))
Procedures
The methodology chosen for this DNP project will be based on the assumption that implementing a peer-led CDSMP for patients with one or more chronic conditions will improve patient outcomes. The project will evaluate a chronic disease self-management peer-led group, called "The Healthy Living Workshop." The Healthy Living Workshop is based off a CDSMP system developed by the Stanford Patient Education Research Center (SPERC). The SPERC is part of the Department of Medicine at Stanford University. The SPERC designs programs that help people manage their health problems, gain self-confidence in their ability to control their symptoms and to lead fuller, healthier lives (Stanford Patient Education Research Center [SPERC], n.d.).
The workshops consist of 6 sessions, one day per week, for 21/2 hours.
Program Content includes:
- Decision-making & problem-solving skills
- Long-term exercise program
- Fatigue management
- Dealing with anger, depression, & other negative emotions
- Cognitive management of pain & stress
- Communication with family, friends, & physicians
- Using prescribed medications
- Healthy eating
- Making informed treatment decisions
- Fall prevention
- Weight management
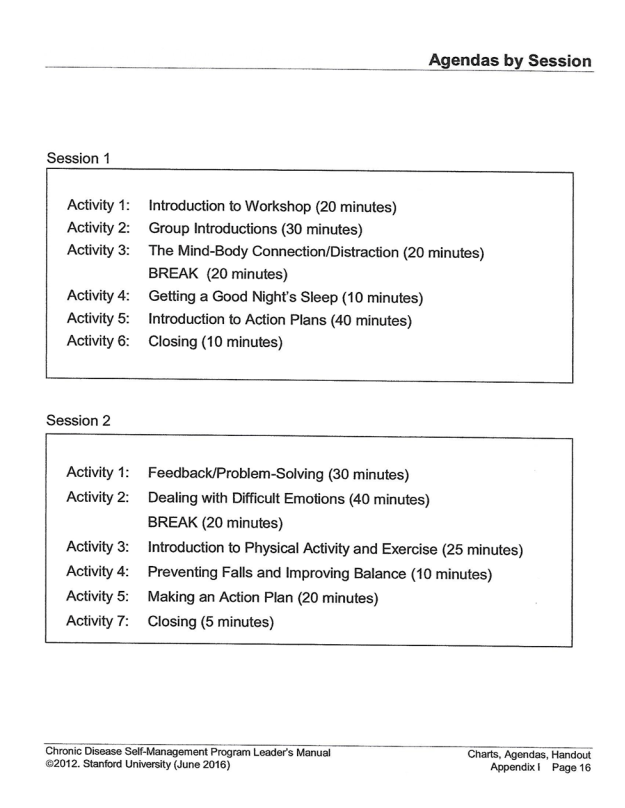
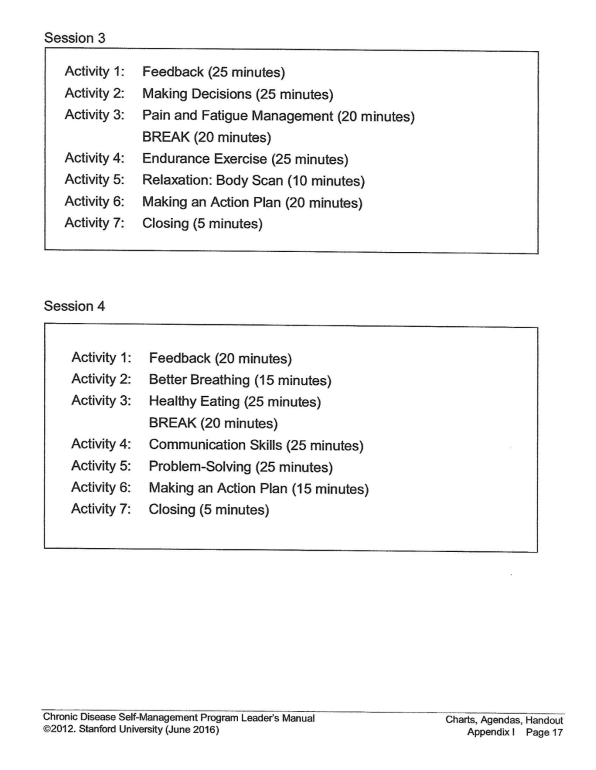
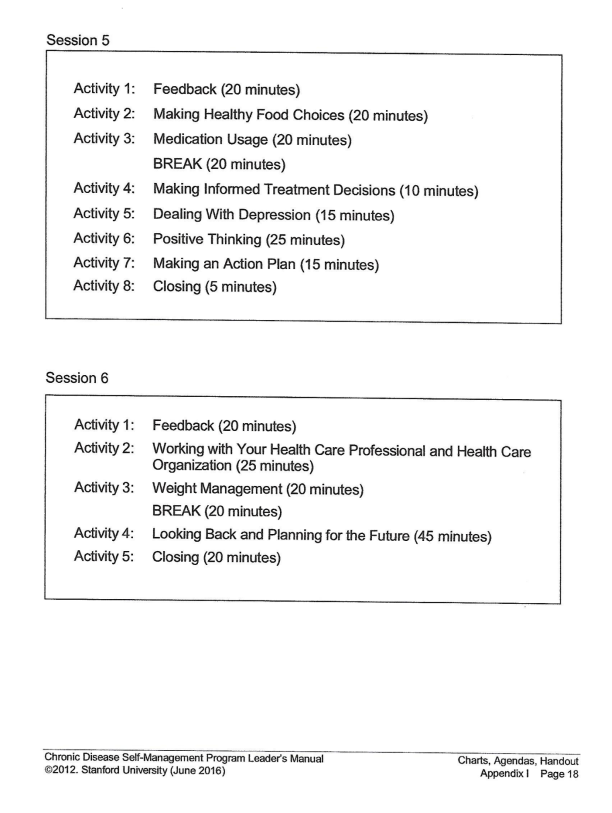
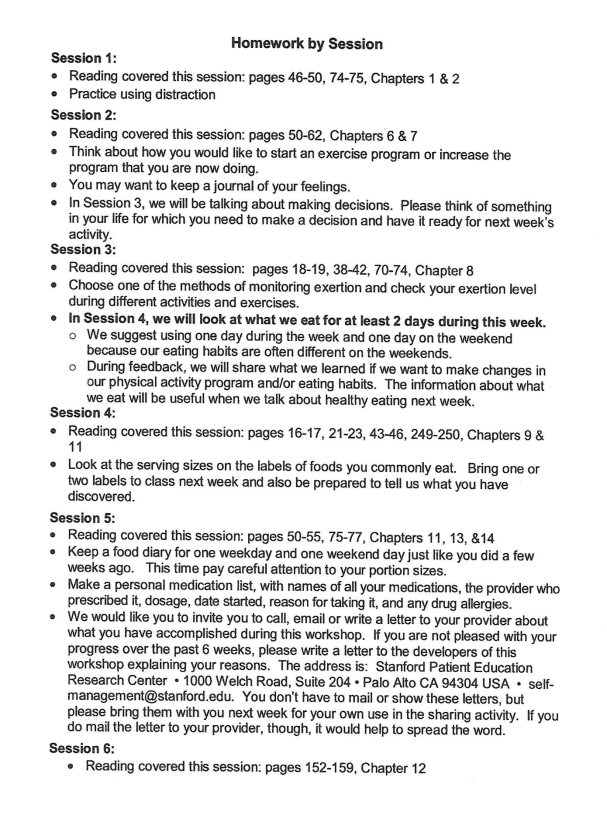
Each session has a structured agenda (Appendix A-C) and homework assigned to facilitate further learning (Appendix D).
(CHAS, 2017)
Setting
The setting for this project will be the Community Health Association of Spokane (CHAS). CHAS Health is a non-profit, federally qualified health center (FQHC) providing first-rate medical, dental, pharmacy, and behavioral health services to families and individuals of all ages, regardless of insurance status. CHAS currently serves approximately 52,000 patients each year throughout Spokane County and the Lewis-Clark Valley. The mission of CHAS is to improve the overall health of the communities they serve by expanding access to quality health and wellness services. As a FQHC, CHAS is a "patient led" organization with 51% of the Board of Directors currently active, registered patients of CHAS. CHAS has 6 clinics and 2 urgent care in the Spokane area. The Healthy Living Workshops are held at various locations across the Spokane area (Community Health Association of Spokane [CHAS], 2017).
Participants
Participants will be between the ages of 18 to 80 years old, with a least one or more chronic conditions (include but not limited to; heart disease, cancer, type 2 diabetes, obesity and arthritis) or the primary care-giver of a patient with one or more chronic conditions. Patient must have attended five of the six Healthy Living Workshops over a six week period to be considered "graduates" of the program. In addition primary care providers and workshop leaders will also be asked to participate in surveys and post-workshop interviews.
Data Collection/Analysis
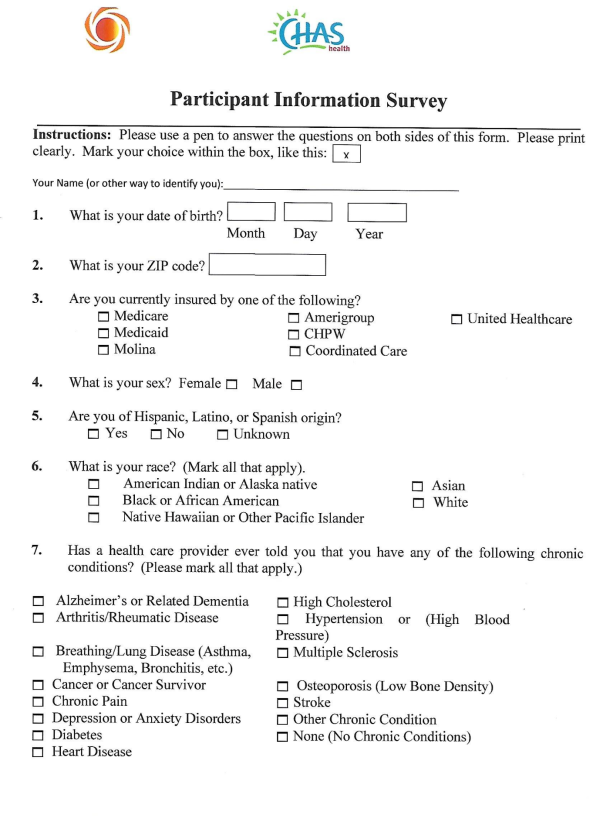
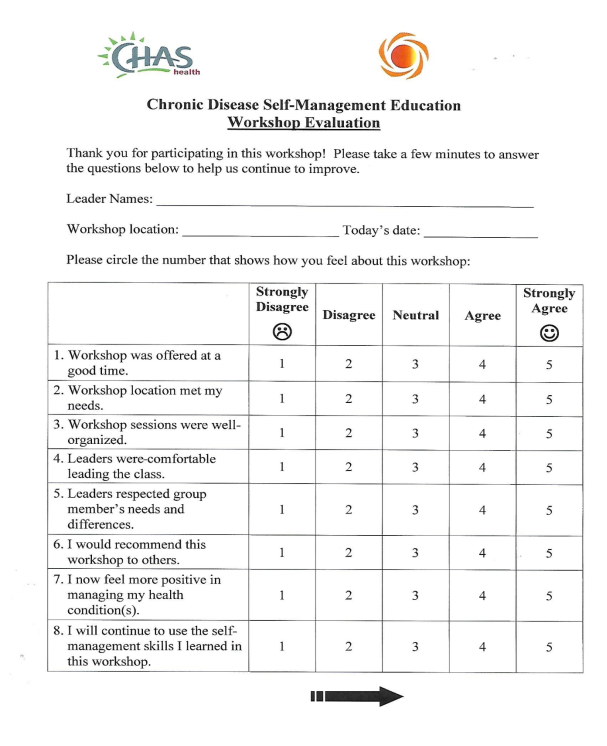
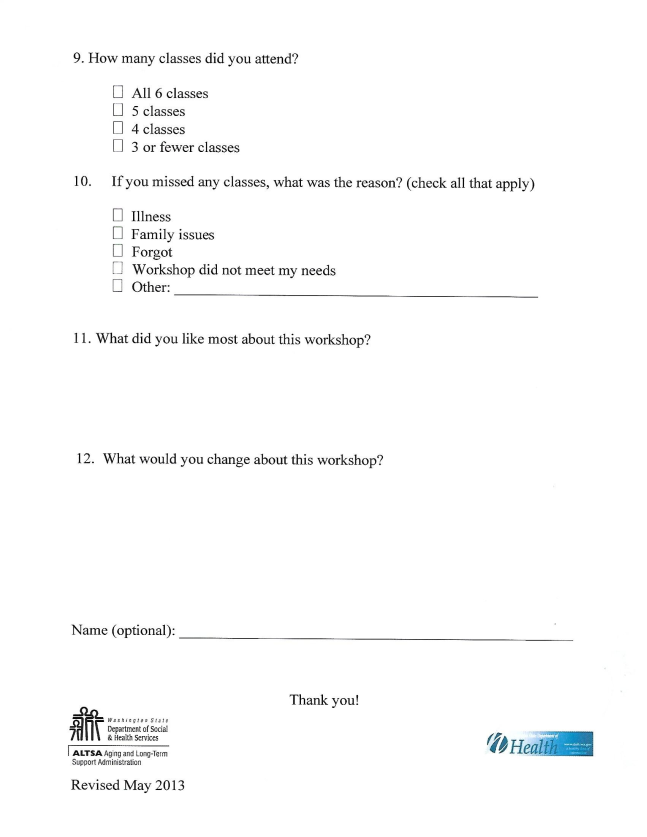
Data interpretation will be accomplished employing an integrative approach using qualitative and quantitative measures. I will participate in the Healthy Living Workshops over a six week period. Demographic data will be collected using CHAS Health Participant Information Survey (Appendix E). A Likert Scale will be utilized for post-workshop evaluation (Appendix G). Post workshop phone interview questions, will be determined at a later date. Phone or in person interviews will be conducted with primary care providers at multiple CHAS clinics in the Spokane Area.
References
Ahn, S., Basu, R., Smith, M. L., Jiang, L., Lorig, K., Whitelaw, N., & Ory, M. G. (2013). The impact of chronic disease self-management programs: Healthcare savings through a community-based intervention. BMC Public Health, 13, 1141. doi:10.1186/1471-2458-13-1141
Ahn, S., Smith, M. L., Altpeter, M., Post, L., & Ory, M. G. (2015). Healthcare cost savings estimator tool for chronic disease self-management program: A new tool for program administrators and decision makers. Frontiers in Public Health, 3 doi:10.3389/fpubh.2015.00042
Basu, R., Ory, M. G., Towne, S. D., Smith, M. L., Hochhalter, A. K., & Ahn, S. (2015). Cost-effectiveness of the chronic disease self-management program: Implications for community-based organizations. Frontiers in Public Health, 3 doi:10.3389/fpubh.2015.00027
Bauer, U. E., Briss, P. A., Goodman, R. A., & Bowman, B. A. (2014) Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. The Lancet, 384(9937), 45-52. doi:10.1016/S0140-6736(14)60648-6
Centers for Disease Control and Prevention. (2012). Chronic Diseases: The Leading Causes of Death and Disability in the United States. Retrieved from https://www.cdc.gov/chronicdisease/overview/index.htm#ref1
Centers for Disease Control and Prevention. (2016). Program Performance and Evaluation Office-Evaluation Standards. Retrieved from https://www.cdc.gov/eval/standards/index.htm
CHAS (2016) Healthy Living Workshops. Retrieved from https://chas.org/services/education
Framework for Program Evaluation [Online Image]. (2016) Retrieved from https://www.cdc.gov/eval/framework/
Innovative Care for Chronic Conditions: Building Blocks for Action [Online Image]. ( 2002) Retrieved from http://www.who.int/diabetes/publications/icccreport/en/
Koplan, Jeffrey P., Wetterhall, Scott F., Milstein, Robert L. (1999). Framework for program evaluation in public health. MMWR. Recommendations and Reports: Morbidity and Mortality Weekly Report. Recommendations and Reports / Centers for Disease Control, 48(RR-11), 1. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10499397
Pruitt, S., Annandalte, S., Epping-Jordan, J., Fernandez Diaz, J., Khan, M., Kisa, A., Klapow, J., Solinis, R., Reddy, S., & Wagner, E. (2002) Innovative Care for Chronic Conditions-Building Blocks for Action. World Health Organization. Retrieved from http://www.who.int/chp/knowledge/publications/icccreport/en/
Stanford Patient Education Research Center (n.d) Chronic Disease Self-Management Program. Retrieved from http://patienteducation.stanford.edu/programs/cdsmp.html
Ward, B.W., Schiller, J.S., & Goodman, R.A. (2014) Multiple Chronic Conditions Among US Adults: A 2012 Update. Preventing Chronic Disease, 2014, 11 (4) DOI: http://dx.doi.org/10.5888/pcd11.130389 .
.
APPENDIX A. WORKSHOP SESSION 1-2
APPENDIX B. WORKSHOP SESSION 3-4
APPENDIX C. WORKSHOP SESSION 5-6
APPENDIX D. HOMEWORK PER SESSIONS
APPENDIX E. PARTICIPANT INFORMATION SURVEY
APPENDIX F. CHRONIC DISEASE SELF MANAGEMENT EDUCATION WORKSHOP EVALUATION
Cite This Work
To export a reference to this article please select a referencing style below:


