FACILITATING THE LEARNING OF SECOND YEAR STUDENT NURSE on SURGICAL SCRUB TECHNIQUE
ABSTRACT
INTRODUCTION
This report is focused on the learning facilitation of a nursing skill to a second-year student nurse. The placement was in the main theatres in a large hospital, hence creating a welcome environment, stabilising a good relationship between the mentor and mentee and introducing the student to the multidisciplinary team, was important to enhance the learning experience.
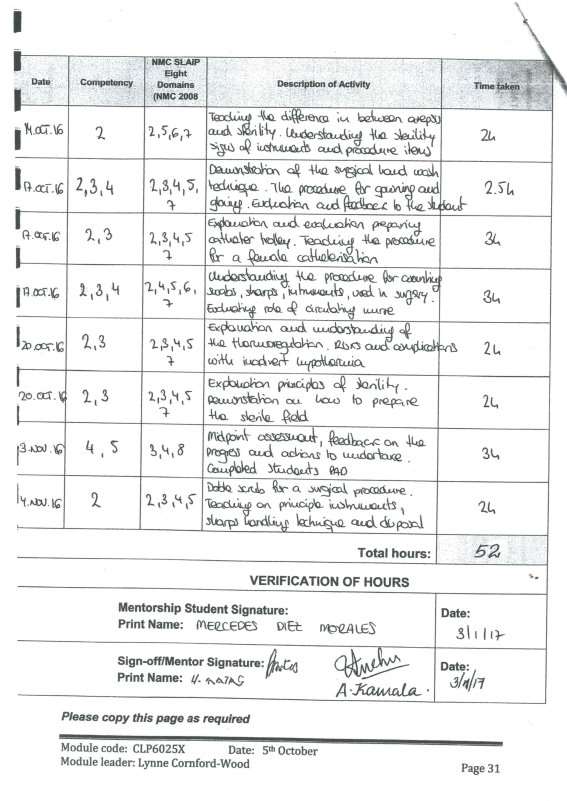
The maintenance of sterility is key in theatres to prevent the contamination of microorganisms throughout the surgical procedure (Phillips, 2013). Hence is basic for the student nurse to learn the surgical scrub technique, which is the process of removing as many microorganisms as possible from the skin of the hands and arms before donning sterile surgical attire (Woodhead and Fudge, 2011). The novice mentor has used a range of facilitative strategies to support learning, covering the second domain in the CAD of mentorship, the evidence is given in the appendix 1. The NMC’s Slaip domains relating to this activity are facilitation of learning, evaluation of learning and evidence based practice.
Get Help With Your Essay
If you need assistance with writing your essay, our professional essay writing service is here to help!
All the students should be keen to learn. There is plenty of information included in the NMC guidelines, hospital policies and nursing text books among others, which will influence the effectiveness of learning. In order to help the student to acquire the skill, the activity was broken down into different stages. The student will learn from observation, as the novice mentor will demonstrate and explained the activity in a sequential order. Therefore, before performing it for a real case, the student nurse will benefit from the experiential learning.
THEORIES, FACILITATION OF LEARNING
The facilitation of learning is the second domain in the NMC’s Standards for supporting learning and assessment in practice (2008, p. 63), which state that the teacher must ‘facilitate learning for a range of students, within a particular area of practice where appropriate, encouraging self-management of learning opportunities and providing support to maximise individual potential’. Additionally, the NMC code (2015) highlight the importance of sharing skills, knowledge and experience with students and colleagues. Undoubtedly, all professionals are involved in the process of helping the healthcare student to achieve their competencies.
Kilgallon and Thompsons (2012) defined the facilitation of learning as an interactive process influenced by external factors, in which a commitment is needed from both parties, mentor and mentee, to enhance the student learning and personal development. Hinchliffe (2009) adds that the mentor must find out the student’s type of learner, this is the key for a successful teaching and facilitating learning.
The learning style is the particular way in which the student tends to respond to a learning experience to be able to achieve it. Honey and Mumford (2000) developed their model based in Kolb’s work, identifying four learning styles; activists, reflectors, theorists and pragmatists. The student tends to be pragmatist, she prefers to know the theoretical information before practice; however, she could change depending on the task to be undertaken. An important role of the mentor is to make the learner understand how this influence in their learning, hence she can change or adapt them depending on the situation (Gopee 2011).
The importance of been aware of the learning style is that the novice mentor will be able to adapt their facilitation to the student’s preferences. The mentor should have a clear understanding of the learning theories, avoiding to adhere to only one. Additionally, Warburton et al, (2016) suggest that using a wide range a challenging and engaging environment will be created to the student. Most of the theories are developed from the three main types; behaviourist, cognitive and humanistic (Kinnell and Hughes 2010, Gopee 2011, Hinchliffe 2009).
The early theories, such as behaviourist and cognitive theories, base the control of the learning in the teacher. While in the later theories, such us constructivist and humanistic, the students are the centre, where they are responsible and actively involve for their learning with help of the mentor, (Knowles et al 2015). Furthermore, it is crucial a good relationship between mentor and mentee and must be based on mutual trust (Bailey-McHale J. and Hart D. 2013). The student is highly active, enthusiastic and curious; hence she will benefit more from a humanistic and constructivism approach.
Baeten et al (2010) suggests that by making the students responsible for their learning will increase their commitment and motivation. Furthermore, Lunyk-Child et al (2001) study found that the students engage in self-directed learning, they might start with negative feelings but ends with confidence and permanent skills. It is required to the mentor to develop the ability to implement the self-directed learning effectively.
ANALYSIS
Kolbs defined the experiential learning as the knowledge created through the experience. The student is exposed to a new experience in the clinical setting, from which she will learn. Therefore, it is essential that the mentor works like a facilitator when planning the practice experience. Warbarton et al (2016) state that the advantage of a plan learning session is the enhancement in the student’s experience.
Prior start the activity, using the intimacy relationship with the mentee, the mentor must consider the student’s knowledge base, practical and theoretical (Gopee 2011). It is identified that she has certain knowledge on the difference between asepsis and sterility but not a full understanding although she has been exposed to few sterile activities, non-surgical related.
Supported by the humanistic perspective, the motivation to learn is derived from the person’s needs, subjective to feelings and the desire to grow (Braungart and Braungart, 2009). The student is proactive searching for information, and hospital policy was provided. Those will help her to gain the base knowledge, of the procedure and the purpose of it, making the student engage with the activity, and increasing the motivation to learn.
In order to support the student to learn the surgical scrub technique, the lesson plan was prepared using as a base the Peyton´s model, developed in 1998, which is divided in four stages. The purpose to use this model as the novice mentor is to engage the student with what she is require to learn and to learn by doing it.
During the first stage the surgical scrub technique is demonstrated with a brief explanation, and only observation from the student. In the second stage the clinical skill is fully demonstrated and explained, divided in steps, furthermore easily understood. The material is provided in a logical sequence. Hinchliffe (2009) points out that in this way the learning is enhanced. Additionally, the student is encouraged to ask questions.
The novice mentor promoted the student to explain the clinical skill, prior doing it by herself. Besides the used of open questioning techniques, will stimulate the student to think (Burnard 2002). For example, why the correct time for the surgical scrub is important? The student points that prolonged time may cause harm to deep dermal layers and short will not remove all the microorganisms (Phillips, 2013). These are the third and fourth stages in the Peyton’s model (1998).
After the activity, time is allocated for an informal meeting, the student is encouraged to reflect on her performance. Knowles (2015) states that what students do, hear and see in a clinical placement can stay at a superficial level, to make it go deeper the mentor needs to stimulate the student to critically analyse their actions and questioning the meaning of the experience.
The student performance needs further development although the steps have been followed correctly, with more practice her technique will improve quickly. The student’s feedback was positive, highlighting the importance of the correct time allocated and the opportunity to learn by doing it.
RECOMMENDATION FOR BEST PRACTICE (CONCLUSION)
The learning facilitation was effective, the student was able to reach the aim of the activity, by using the Peyton’s model (1998), the novice mentor can ensure the student knows the steps and the rationale of the nursing skill before the practice.
Another model that could have been used is the Steinaker and Bell Experiential Taxonomy, developed in 1979, which identify five levels; from exposure, through participation, identification, internalisation to dissemination. That methodology was not implemented because the tight timelines and it would not fit in this mentor activity. The last two stages require a higher degree of seniority and the student will not have it until she is registered as a nurse with experience.
The theatre is a challenging and busy area, planning the lesson, creating a positive environment, allocating the time and the material needed prior start the activity was essential. The advantage of planning learning sessions is the enhancement of the student’s experience of the placement, giving a clear understanding of what is required from them (Warburton et at, 2016).
It is important to consolidate the learning, after the activity the mentor encourage the student to self-evaluate. Additionally, on other occasion more information is retained, by making the student to teach the clinical skill to a junior student while the mentor evaluates (Walsh, 2014).
REFERENCES
Baeten M., Kyndt E., Struyven K., and Dochy F. (2010) Using student-centred learning environments to stimulate deep approaches to learning: factors encouraging or discouraging their effectiveness. Educational Research Review. 5, 3, 243-160
Bailey-McHale and Hart, D. (2013) Mastering mentorship. A Practical Guide for Mentors of Nursing, Health and Social Care Students. London: SAGE publications Ltd.
Braungart and Braungart (2009) Applying learning theories to healthcare practice. Chapter 3. Available at: http://www.jblearning.com/samples/0763751375/chapter2.pdf (last access: )
Gopee N. (2011) Mentoring and Supervision in Healthcare. Second edition. Sage Publications, London.
Hinchliffe S. (2009) The Practitioner as Teacher. Fourth edition. Edinburgh: Churchill Livingstone Elsevier.
Kilgallon K. and Thompson J. (2012) Mentoring in Nursing and Healthcare: A Practical Approach. John Wiley & Sons, Chichester.
Kinnell D. and Hughes P. (2010) Mentoring Nursing and Healthcare Students. London: SAGE.
Knowles M., Holton E. and Swanson R. (2015) The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development. Eighth edition. Abingdon, Oxon: Routledge.
Lunyk-Child O. L., Crooks D., Ellis P. J., Ofosu C., O’Mara L., and Rideout E. (2001) Self-directed learning: Faculty and student perceptions. Journal of Nursing Education. 40, 3, 116-123.
Nursing and Midwifery Council (2008) Standards to Support Learning and Assessment in Practice. NMC Standards for Mentors, Practice Teachers and Teachers. tinyurl.com/gn82s2m (Last accessed: ).
Nursing and Midwifery Council (NMC) (2008) The Code: Standards of conduct, performance and ethics for nurses and midwives. London: NMC.
Walsh, D. (2014) The nurse mentor’s handbook: supporting students in clinical practice. 2nd edn Maidenhead: McGraw-Hill/Open University Press
Warburton T., Houghton T. and Barry D. (2016) Facilitation of learning: part 1. Nursing Standard. 30, 32, 40-47.
Warburton T., Houghton T. and Barry D. (2016) Facilitation of learning: part 2. Nursing Standard. 30, 35, 41-48.
Woodhead K. and Fudge L. (2012) Manual of Perioperative Care: An Essential Guide. Chichester, West Sussex: Wiley-Blackwell.
http://www.businessballs.com/kolblearningstyles.htm
Appendix 1
Cite This Work
To export a reference to this article please select a referencing style below:


